Health
Hospital wants to pull the plug on inhumanely neglected 23-year-old woman who is not brain dead

From LifeSiteNews
Montefiore Hospital in Brooklyn is neglecting Amber Ebanks, but experts who have seen the student say her body is functioning and that she could improve with proper treatment.
Amber Ebanks, a 23-year-old Jamaican business student, drove herself to Montefiore Hospital in the Bronx for elective surgery on July 30. But her procedure went awry, leading to an intraoperative stroke and brain swelling that worsened over time. Now, her family is fighting for Amber’s life while the hospital wants to pull the plug.
In February, Amber was found to have a ruptured arteriovenous malformation (AVM), a tangle of abnormal arteries and veins in her brain. Thankfully, after the rupture she was able to return to life as normal. Her doctors recommended that she undergo an embolization procedure to clot off the abnormal blood vessels in her brain in hopes of preventing further rupturing and brain damage. Unfortunately, during the embolization procedure, one of the major arteries supplying blood to Amber’s brain was unintentionally occluded, and her procedure was also complicated by a type of bleeding around the brain called a subarachnoid hemorrhage. Thus, she was taken to the ICU, placed in a medically induced coma, and treated for brain swelling.
Just 10 days later, on August 9, her doctors declared her to be “brain dead.” But there were problems with this diagnosis. The Determination of Death statute in New York and the Uniform Determination of Death Act (UDDA) both state:
“An individual who has sustained either:
- irreversible cessation of circulatory and respiratory functions; or
- irreversible cessation of all functions of the entire brain, including the brain stem, is dead.”
Amber Ebanks meets neither the first nor the second of these criteria. Her circulatory and respiratory functions continue: her heart is still beating, and her lungs are absorbing oxygen and releasing carbon dioxide. And she does not have the irreversible cessation of all functions of her brain, since she is maintaining her own body temperature, which is a brain function.
Moreover, the new 2023 American Academy of Neurology brain death guideline indicates that metabolic derangements such as high serum sodium levels may confound a brain death evaluation. According to Dr. Paul Byrne, Amber’s sodium levels were very high prior to her brain death determination, with readings over 160meq/L (normal sodium levels range from 135-145 meq/L). Not only can high sodium levels cause abnormal brain functioning, but they can also cause blood vessels in the brain to rupture, causing more brain bleeding – the very problems that Amber’s doctors should be interested in preventing. Also, even though high levels of carbon dioxide are known to exacerbate brain swelling, her doctors have not been checking these levels or adjusting her ventilator settings to prevent such derangements.
In addition to her ongoing heart, lung, and brain functions, Amber has continuing liver and kidney function. And presumably she still has digestive function, even though the hospital has been refusing to feed her since she came in for her surgery on July 30th. A patient cannot be expected to improve neurologically without nutrition.
Not only is Montefiore Hospital refusing to feed Amber, it’s refusing to provide her with basic wound care and hygiene. When Dr. Byrne, a board-certified pediatrician and neonatologist and brain death expert, flew to New York to see Amber this past week, Amber’s sister Kay showed him a maggot she had removed from her sister’s hair. Referring to hospital personnel, Kay Ebanks said in an ABC News article, “They are some of the cruelest people I have ever known.” Most of Amber’s family lives in Jamaica, and her father has been struggling to get a visa in order to come and see his daughter. Meanwhile, the hospital actually suggested that family members say goodbye to her over the phone.
Dr. Byrne and Dr. Thomas M. Zabiega, a board-certified psychiatrist and neurologist, have both evaluated Amber’s case. They have submitted sworn affidavits that Amber Ebanks is alive, and believe that she has decreased blood flow to her brain causing a quietness of the brain known as Global Ischemic Penumbra (GIP). During GIP, the brain shuts down its function to save energy, but the brain tissue itself remains viable. Drs. Byrne and Zabiega recommend additional time and treatment such as adjusting Amber’s sodium and carbon dioxide levels and treating hormonal deficiencies. They have testified that with proper medical treatments she is likely to continue to live and may obtain limited to full recovery of brain functions, even possibly recovering consciousness.
And there are other health care professionals who are willing to help Amber heal. A long-term care facility on Long Island called New Beginnings has agreed to care for Ebanks for as long as her family would like. “Everybody needs hope. You can’t just give up. Can’t just take them off life support when she needs more time,” New Beginnings founder Allyson Scerri said.
Nevertheless, doctors at Montefiore Hospital are adamant that Amber is “brain dead” and want to disconnect her from her ventilator over the objections of her family. Despite the testimony of qualified doctors and experts, the judge assigned to her case is requiring that a New York-licensed physician be found to evaluate Amber and give testimony about her condition. Until then, Amber remains unfed, uncared for, and neglected in an American hospital, to the point of her sister having to remove vermin from her hair.
Amber Ebanks is very much alive despite receiving little to no ongoing treatment to assist with the healing of her brain. She does not meet the medical or legal criteria for death. All she needs are proper ventilator therapy, a balancing of her fluids and electrolytes, nutrition via a feeding tube, and hormonal replacement: treatments that are commonplace in medicine today. It is shameful that her family has had to beg for these treatments and even go to court to try to force the hospital to provide them.
Heidi Klessig, MD is a retired anesthesiologist and pain management specialist who writes and speaks on the ethics of organ harvesting and transplantation. She is the author of “The Brain Death Fallacy” and her work may be found at respectforhumanlife.com.
Health
FDA warns ‘breast binder’ manufacturers to stop marketing to gender-confused girls

From LifeSiteNews
Dr. Marty Makary took aim at the transgender-medical-industrial complex that has exploded in recent years during a recent press conference.
Food and Drug Administration (FDA) commissioner Dr. Marty Makary has sternly warned companies manufacturing “breast binders” to cease marketing and supplying their product to gender-confused girls seeking to make their bodies appear masculine.
“Today the FDA is taking action,” said Makary in a press conference. “We are sending warning letters to 12 manufacturers and retailers for illegal marketing of breast binders for children, for the purposes of treating gender dysphoria.”
“Breast binders are a class one medical device with legitimate medical users, such as being used by women after breast cancer surgery,” but “these binders are not benign,” he cautioned. “Long-term usage has been associated with pain, compromised lung function, and even difficulty breast feeding later in life.”
“The warning letters will formally notify the companies of their significant regulatory violations and require prompt corrective action,” said the FDA head.
.@DrMakaryFDA: “Today the FDA is taking action. We are sending warning letters to 12 manufacturers and retailers for illegal marketing of breast binders for children, for the purposes of treating gender dysphoria.” pic.twitter.com/6JNAy36223
— HHS Rapid Response (@HHSResponse) December 18, 2025
The warning letter addressed to California manufacturer, GenderBender, notes that the company’s website states that “[c]hest binding is the practice of compressing breast mass into a more masculine shape, often done in the LGBTQ community for gender euphoria.”
“Your firm should take prompt action to address any violations identified in this letter. Failure to adequately address this matter may result in regulatory action being initiated by the FDA without further notice. These actions include, but are not limited to, seizure and injunction,” advised the FDA.
During his presentation, Makary took aim at the transgender-medical-industrial complex that has exploded in recent years.
“One of the most barbaric features of a society is the genital mutilation of its children,” observed Makary.
“Pushing transgender ideology in children is predatory, it’s wrong, and it needs to stop,” he declared.
“This ideology is a belief system that some teachers, some pediatricians, and others are selling to children without their parents knowing sometimes, or with a deliberate attempt to remove parents from the decision making,” Makary explained.
To witness society “putting kids on a path of chest binders, drugs, castration, mastectomies, and other procedures is a path that now many kids regret,” he lamented, as he pointed to Chloe Cole, who has reverted to her God-given femininity after undergoing so-called “gender-affirming” surgery as a teen.
Cole is a leading voice for young people who have “detransitioned” after having medically, surgically, and socially attempted to “transition” to a member of the opposite sex.
.@DrMakaryFDA: “Pushing transgender ideology in children is predatory, it's wrong, and it needs to stop.” pic.twitter.com/TXxWNEtNZk
— HHS Rapid Response (@HHSResponse) December 18, 2025
Health
All 12 Vaccinated vs. Unvaccinated Studies Found the Same Thing: Unvaccinated Children Are Far Healthier

I joined Del Bigtree in studio on The HighWire to discuss what the data now make unavoidable: the CDC’s 81-dose hyper-vaccination schedule is driving the modern epidemics of chronic disease and autism.
This was not a philosophical debate or a clash of opinions. We walked through irrefutable, peer-reviewed evidence showing that whenever vaccinated and unvaccinated children are compared directly, the unvaccinated group is far healthier—every single time.
Reanalyzing the Largest Vaccinated vs. Unvaccinated Birth-Cohort Study Ever Conducted
At the center of our discussion was our peer-reviewed reanalysis of the Henry Ford Health System vaccinated vs. unvaccinated birth-cohort study (Lamerato et al.)—the largest and most rigorous comparison of its kind ever conducted.
|
The original authors relied heavily on Cox proportional hazards models, a time-adjusted approach that can soften absolute disease burden. Even so, nearly all chronic disease outcomes were higher in vaccinated children.
Our reanalysis used direct proportional comparisons, stripping away the smoothing and revealing the full magnitude of the signal.
- All 22 chronic disease categories favored the unvaccinated cohort when proportional disease burden was examined
- Cancer incidence was 54% higher in vaccinated children (0.0102 vs. 0.0066)
- When autism-associated conditions were grouped appropriately—including autism, ADHD, developmental delay, learning disability, speech disorder, neurologic impairment, seizures, and related diagnoses—the vaccinated cohort showed a 549% higher odds of autism-spectrum–associated clinical outcomes
The findings are internally consistent, biologically coherent, and concordant with every prior vaccinated vs. unvaccinated study, all of which show drastically poorer health outcomes among vaccinated children
The 12 Vaccinated vs. Unvaccinated Studies Regulators Ignore
In the McCullough Foundation Autism Report, we compiled all 12 vaccinated vs. unvaccinated pediatric studies currently available. These studies span different populations, countries, study designs, and data sources.
Every single one reports the same overall pattern. Across all 12 studies, unvaccinated children consistently exhibit substantially lower rates of chronic disease, including:
- Autism and other neurodevelopmental disorders
- ADHD, tics, learning and speech disorders
- Asthma, allergies, eczema, and autoimmune conditions
- Chronic ear infections, skin disorders, and gastrointestinal illness
This level of consistency across independent datasets is precisely what epidemiology looks for when assessing causality. It also explains why no federal agency has ever conducted—or endorsed—a fully vaccinated vs. fully unvaccinated safety study.
Flu Shot Failure
We also addressed the persistent failure of seasonal influenza vaccination.
A large Cleveland Clinic cohort study of 53,402 employees followed participants during the 2024–2025 respiratory viral season and found:
- 82.1% of employees were vaccinated against influenza
- Vaccinated individuals had a 27% higher adjusted risk of influenza compared with the unvaccinated state (HR 1.27; 95% CI 1.07–1.51; p = 0.007)
- This corresponded to a negative vaccine effectiveness of −26.9% (95% CI −55.0 to −6.6%), meaning vaccination was associated with increased—not reduced—risk of influenza
When vaccination exposure increases, chronic disease, neurodevelopmental disorders, and inflammatory illness increase with it. When children are unvaccinated, they are measurably healthier across virtually every outcome that matters.
The science needed to confront the chronic disease and autism epidemics already exists. What remains is the willingness to acknowledge it.
Epidemiologist and Foundation Administrator, McCullough Foundation
Support our mission: mcculloughfnd.org
Please consider following both the McCullough Foundation and my personal account on X (formerly Twitter) for further content.
FOCAL POINTS (Courageous Discourse) is a reader-supported publication.
To receive new posts and support my work, consider becoming a free or paid subscriber.
-

 Censorship Industrial Complex22 hours ago
Censorship Industrial Complex22 hours agoDeath by a thousand clicks – government censorship of Canada’s internet
-

 Daily Caller23 hours ago
Daily Caller23 hours agoChinese Billionaire Tried To Build US-Born Baby Empire As Overseas Elites Turn To American Surrogates
-

 Great Reset1 day ago
Great Reset1 day agoViral TikTok video shows 7-year-old cuddling great-grandfather before he’s euthanized
-

 Automotive1 day ago
Automotive1 day agoPoliticians should be honest about environmental pros and cons of electric vehicles
-

 Digital ID21 hours ago
Digital ID21 hours agoCanada releases new digital ID app for personal documents despite privacy concerns
-

 Community18 hours ago
Community18 hours agoCharitable giving on the decline in Canada
-

 Alberta24 hours ago
Alberta24 hours agoSchools should go back to basics to mitigate effects of AI
-
 Bruce Dowbiggin20 hours ago
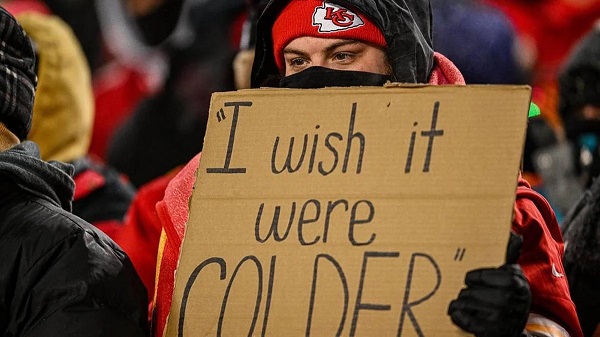
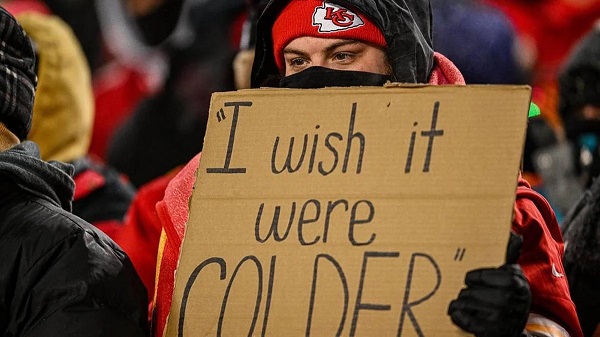
Bruce Dowbiggin20 hours agoNFL Ice Bowls Turn Down The Thermostat on Climate Change Hysteria







