Alberta
Canada’s health-care wait times hit 27.7 weeks in 2023—longest ever recorded

From the Fraser Institute
By Mackenzie Moir and Bacchus Barua
Canadian patients waited longer than ever this year for medical treatment, finds a new study released by the Fraser Institute, an independent, non-partisan Canadian public policy think-tank.
The study, an annual survey of physicians across Canada, reports a median wait time of 27.7 weeks—the longest ever recorded, longer than the wait of 27.4 weeks reported in 2022—and 198 per cent higher than the 9.3 weeks Canadians waited in 1993, when the Fraser Institute began tracking wait times.

“COVID-19 and related hospital closures have exacerbated, but are not the cause, of Canada’s historic wait times challenges,” said Bacchus Barua, director of the Fraser Institute’s Centre for Health Policy Studies and co-author of Waiting Your Turn: Wait Times for Health Care in Canada, 2023.
“Previous results revealed that patients waited an estimated 20.9 weeks for medically necessary elective care in 2019—long before the pandemic started.”
The study examines the total wait time faced by patients across 12 medical specialties from referral by a general practitioner (i.e. family doctor) to consultation with a specialist, to when the patient ultimately receives treatment.
More than 1,200 responses were received across the 12 specialties and 10 provinces. Among the provinces, Ontario recorded the shortest wait time at 21.6 weeks—still up from 20.3 weeks in 2022. Nova Scotia recorded the longest wait time in Canada at 56.7 weeks.
Among the various specialties, national wait times were longest between a referral by a GP and plastic (52.4 weeks), orthopedic (44.3) neurosurgery (43.5). Wait times were shortest for radiation (4.4 weeks) and medical oncology treatments (4.8 weeks). Patients also experience significant waiting times for various diagnostic technologies. This year, Canadians could expect to wait 6.6 weeks for a computed tomography (CT) scan, 12.9 weeks for a magnetic resonance imaging (MRI) scan, and 5.3 weeks for an ultrasound.
Crucially, physicians report that their patients are waiting over four and a half weeks longer for treatment (after seeing a specialist) than what they consider to be clinically reasonable.
“Excessively long wait times remain a defining characteristic of Canada’s health-care system” said Mackenzie Moir, Fraser Institute policy analyst and co-author of the report. “And they aren’t simply minor inconveniences, they can result in increased suffering for patients, lost productivity at work, a decreased quality of life, and in the worst cases, disability or death.”
Median wait times by province (in weeks)
PROVINCE 2022 2023
British Columbia 25.8 27.7
Alberta 33.3 33.5
Saskatchewan 30.1 31.0
Manitoba 41.3 29.1
Ontario 20.3 21.6
Quebec 29.4 27.6
New Brunswick 43.3 52.6
Nova Scotia 58.2 56.7
P.E.I. 64.7 55.2
Newfoundland and Labrador 32.1 33.3

Each year, the Fraser Institute surveys physicians across twelve specialties and the ten provinces in order to document the queues for visits to specialists and for diagnostic and surgical procedures in Canada. Waiting Your Turn: Wait Times for Health Care in Canada, 2023 Report reports the results of this year’s survey.
In 2023, physicians report a median wait time of 27.7 weeks between a referral from a general practitioner and receipt of treatment. This represents the longest delay in the survey’s history and is 198% longer than the 9.3 weeks Canadian patients could expect to wait in 1993.
Overall, Ontario reports the shortest wait across Canada (21.6 weeks) while Nova Scotia had the longest (56.7 weeks).
The 27.7 week total wait time that patients face can be examined in two consecutive segments:
- referral by a general practitioner to consultation with a specialist: 14.6 weeks;
- consultation with a specialist to receipt of treatment: 13.1 weeks.
After seeing a specialist, Canadian patients were waiting 4.6 weeks longer than what physicians consider clinically reasonable (8.5 weeks).
Across the ten provinces, the study also estimates that there were 1,209,194 procedures for which patients—3% of the Canadian population—were waiting in 2023.
Patients also face considerable delays for diagnostic technology. This year, Canadians could expect to wait 6.6 weeks for a CT scan, 12.9 for an MRI scan, and 5.3 weeks for an ultrasound.
Survey results suggest that, despite provincial strategies to reduce wait times, Canadian patients continue to wait too long for medically necessary treatment.
Data were collected from the week of January 16 to July 1, 2023, longer than the period of collection in years before the COVID19 pandemic. A total of 1,269 responses were received across the 12 specialties surveyed. However, this year’s response rate was 10.3% (lower than in some previous years). As a result, the findings in this report should be interpreted with caution.
Research has repeatedly indicated that wait times for medically necessary treatment are not benign inconveniences. Wait times can, and do, have serious consequences such as increased pain, suffering, and mental anguish. In certain instances, they can also result in poorer medical outcomes—
transforming potentially reversible illnesses or injuries into chronic, irreversible conditions, or even permanent disabilities. In many instances, patients may also have to forgo their wages while they wait for treatment, resulting in an economic cost to the individuals themselves and the economy in general.
The results of this year’s survey indicate that despite provincial strategies to reduce wait times and high levels of health expenditure, it is clear that patients in Canada continue to wait too long to receive medically necessary treatment.
Waiting Your Turn: Wait Times for Health Care in Canada, 2023 Report
By Mackenzie Moir and Bacchus Barua, with Hani Wannamaker
www.fraserinstitute.org
Authors:
Alberta
Alberta’s move to ‘activity-based funding’ will improve health care despite naysayer claims

From the Fraser Institute
After the Smith government recently announced its shift to a new approach for funding hospitals, known as “activity-based funding” (ABF), defenders of the status quo in Alberta were quick to argue ABF will not improve health care in the province. Their claims are simply incorrect. In reality, based on the experiences of other better-performing universal health-care systems, ABF will help reduce wait times for Alberta patients and provide better value-for-money for taxpayers.
First, it’s important to understand Alberta is not breaking new ground with this approach. Other developed countries shifted to the ABF model starting in the early 1990s.
Indeed, after years of paying their hospitals a lump-sum annual budget for surgical care (like Alberta currently), other countries with universal health care recognized this form of payment encouraged hospitals to deliver fewer services by turning each patient into a cost to be minimized. The shift to ABF, which compensates hospitals for the actual services they provide, flips the script—hospitals in these countries now see patients as a source of revenue.
In fact, in many universal health-care countries, these reforms began so long ago that some are now on their second or even third generation of ABF, incorporating further innovations to encourage an even greater focus on quality.
For example, in Sweden in the early 1990s, counties that embraced ABF enjoyed a potential cost savings of 13 per cent over non-reforming counties that stuck with budgets. In Stockholm, one study measured an 11 per cent increase in hospital activity overall alongside a 1 per cent decrease in costs following the introduction of ABF. Moreover, according to the study, ABF did not reduce access for older patients or patients with more complex conditions. In England, the shift to ABF in the early to mid-2000s helped increase hospital activity and reduce the cost of care per patient, also without negatively affecting quality of care.
Multi-national studies on the shift to ABF have repeatedly shown increases in the volume of care provided, reduced costs per admission, and (perhaps most importantly for Albertans) shorter wait times. Studies have also shown ABF may lead to improved quality and access to advanced medical technology for patients.
Clearly, the naysayers who claim that ABF is some sort of new or untested reform, or that Albertans are heading down an unknown path with unmanageable and unexpected risks, are at the very least uninformed.
And what of those theoretical drawbacks?
Some critics claim that ABF may encourage faster discharges of patients to reduce costs. But they fail to note this theoretical drawback also exists under the current system where discharging higher-cost patients earlier can reduce the drain on hospital budgets. And crucially, other countries have implemented policies to prevent these types of theoretical drawbacks under ABF, which can inform Alberta’s approach from the start.
Critics also argue that competition between private clinics, or even between clinics and hospitals, is somehow a bad thing. But all of the developed world’s top performing universal health-care systems, with the best outcomes and shortest wait times, include a blend of both public and private care. No one has done it with the naysayers’ fixation on government provision.
And finally, some critics claim that, under ABF, private clinics will simply focus on less-complex procedures for less-complex patients to achieve greater profit, leaving public hospitals to perform more complex and thus costly surgeries. But in fact, private clinics alleviate pressure on the public system, allowing hospitals to dedicate their sophisticated resources to complex cases. To be sure, the government must ensure that complex procedures—no matter where they are performed—must always receive appropriate levels of funding and similarly that less-complex procedures are also appropriately funded. But again, the vast and lengthy experience with ABF in other universal health-care countries can help inform Alberta’s approach, which could then serve as an example for other provinces.
Alberta’s health-care system simply does not deliver for patients, with its painfully long wait times and poor access to physicians and services—despite its massive price tag. With its planned shift to activity-based funding, the province has embarked on a path to better health care, despite any false claims from the naysayers. Now it’s crucial for the Smith government to learn from the experiences of others and get this critical reform right.
2025 Federal Election
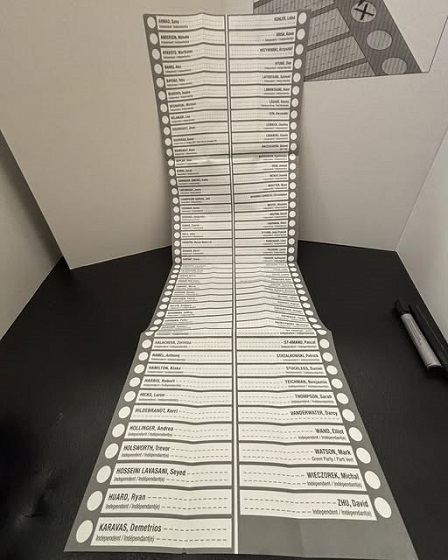
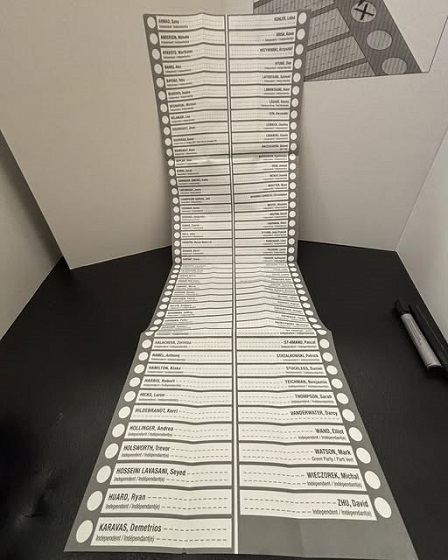
Group that added dozens of names to ballot in Poilievre’s riding plans to do it again
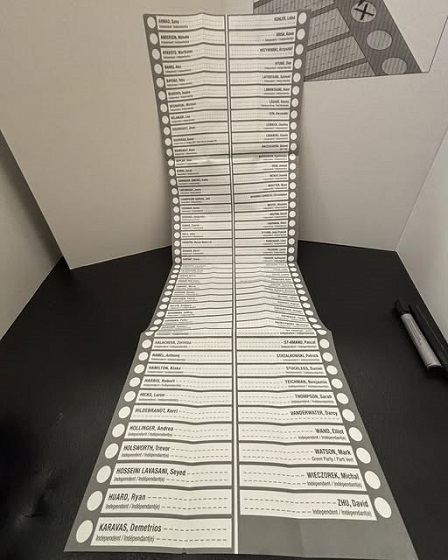
From LifeSiteNews
The ‘Longest Ballot Committee’ is looking to run hundreds of protest candidates against Conservative leader Pierre Poilievre in an upcoming by-election in the Alberta.
A group called the “Longest Ballot Committee” is looking to run hundreds of protest candidates against Conservative Party leader Pierre Poilievre in an upcoming by-election in the Alberta Battle River–Crowfoot riding, just like they did in his former Ottawa-area Carelton riding in last week’s election.
The Longest Ballot Committee is a grassroots group that packs ridings with protest candidates and is looking to place 200 names in the Battle River–Crowfoot riding. The riding was won by Conservative-elect MP Damien Kurek who garnered over 80 percent of the vote, but has since said he is going to vacate his seat to allow Poilievre to run a by-election and reclaim his seat in Parliament in a Conservative-safe area.
In an email to its followers, the committee said “dozens and dozens” of volunteers are ready to sign up as candidates for the yet-to-be-called by-election. The initiative follows after the group did the same thing in Poilievre’s former Carelton riding which he lost last Monday, and which saw voters being given an extremely long ballot with 90 candidates.
The group asked people who want to run to send them their legal name and information by May 12, adding that if about 200 people sign up they will “make a long ballot happen.”
-

 International2 days ago
International2 days agoIce Surprises – Arctic and Antarctic Ice Sheets Are Stabilizing and Growing
-

 Alberta2 days ago
Alberta2 days agoEnergy projects occupy less than three per cent of Alberta’s oil sands region, report says
-

 Energy2 days ago
Energy2 days agoCarney’s energy superpower rhetoric falls flat without policy certainty
-

 Energy2 days ago
Energy2 days agoOil tankers in Vancouver are loading plenty, but they can load even more
-
 2025 Federal Election2 days ago
2025 Federal Election2 days agoGroup that added dozens of names to ballot in Poilievre’s riding plans to do it again
-

 Alberta2 days ago
Alberta2 days agoCharges laid in record cocaine seizure
-

 2025 Federal Election2 days ago
2025 Federal Election2 days agoCarney says Liberals won’t make voting pact with NDP
-
 Autism1 day ago
Autism1 day agoNIH, CMS partner on autism research









